- Calcium & bone metabolism
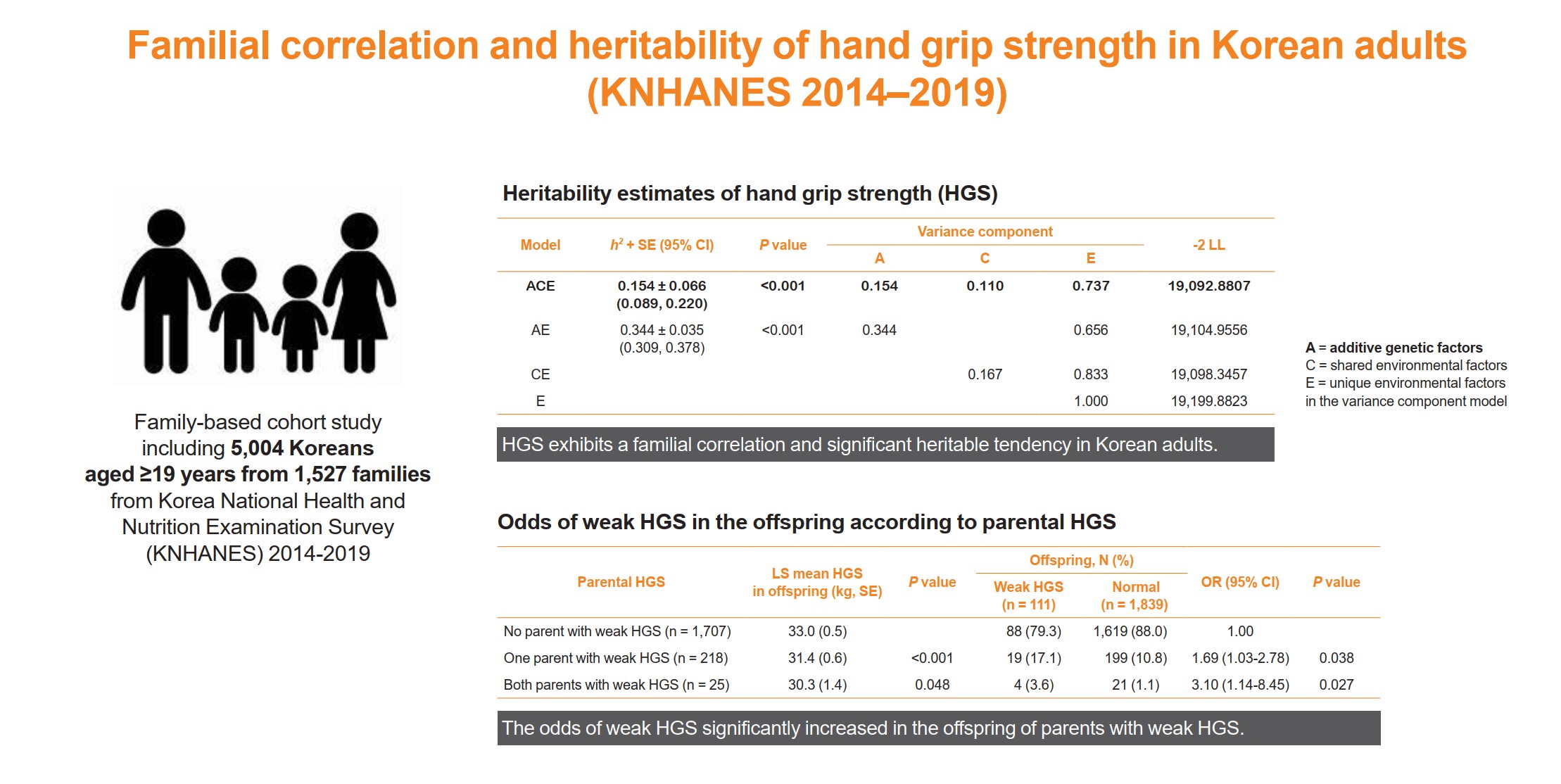
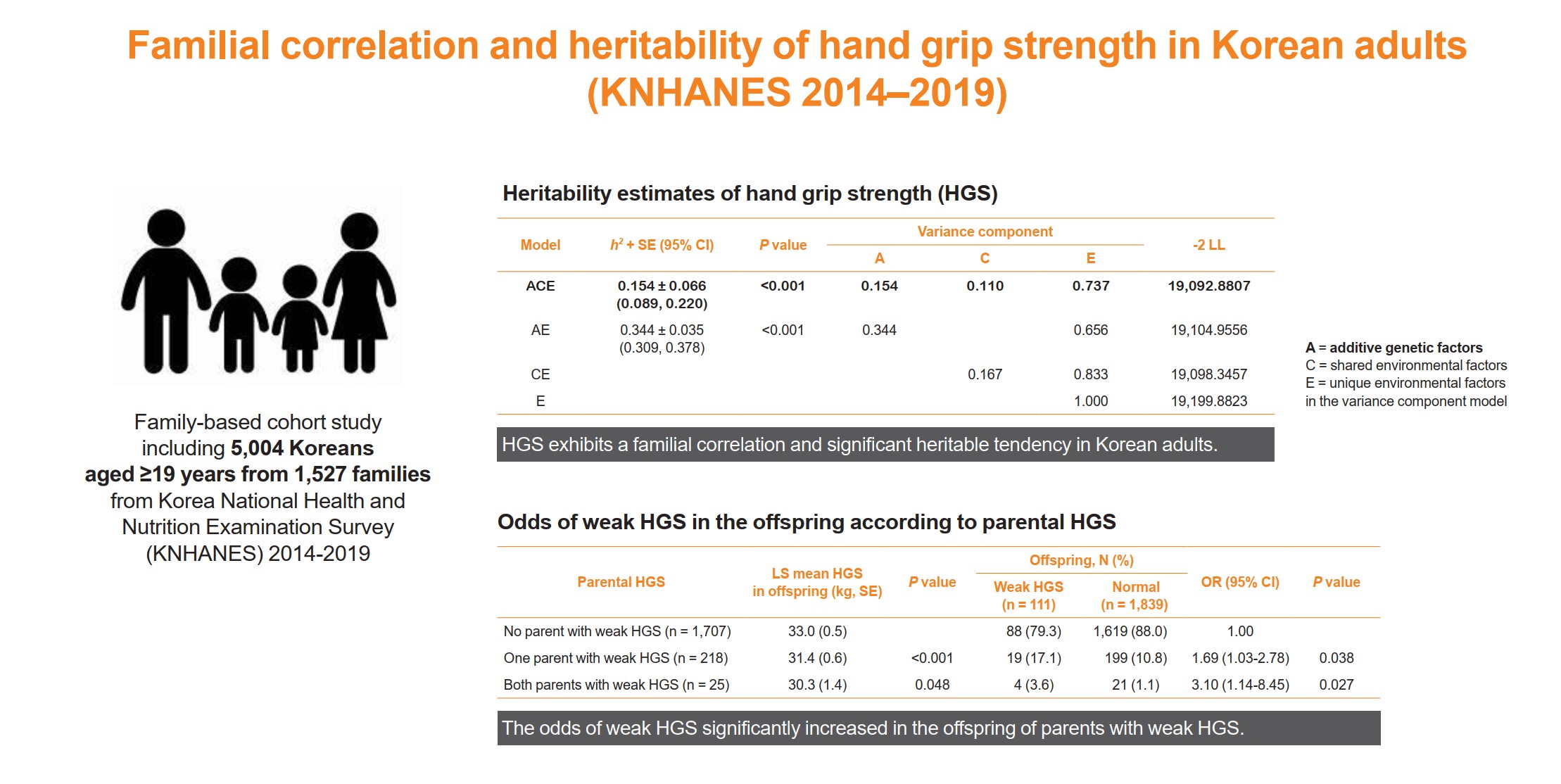
- Familial Correlation and Heritability of Hand Grip Strength in Korean Adults (Korea National Health and Nutrition Examination Survey 2014 to 2019)
-
Seong Hee Ahn, Eun Byeol Park, Seongha Seo, Yongin Cho, Da Hea Seo, So Hun Kim, Young Ju Suh, Seongbin Hong
-
Endocrinol Metab. 2023;38(6):709-719. Published online November 7, 2023
-
DOI: https://doi.org/10.3803/EnM.2023.1740
-
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader  ePub ePub
- Background
The onset and progression of sarcopenia are highly variable among individuals owing to genetic and environmental factors. However, there are a limited number of studies measuring the heritability of muscle strength in large numbers of parent-adult offspring pairs. We aimed to investigate the familial correlation and heritability of hand grip strength (HGS) among Korean adults.
Methods
This family-based cohort study on data from the Korea National Health and Nutrition Examination Survey (2014 to 2019) included 5,004 Koreans aged ≥19 years from 1,527 families. HGS was measured using a digital grip strength dynamometer. Familial correlations of HGS were calculated in different pairs of relatives. Variance component methods were used to estimate heritability.
Results
The heritability estimate of HGS among Korean adults was 0.154 (standard error, 0.066). Correlation coefficient estimates for HGS between parent-offspring, sibling, and spouse pairs were significant at 0.07, 0.10, and 0.23 (P<0.001, P=0.041, and P<0.001, respectively). The total variance in the HGS phenotype was explained by additive genetic (15.4%), shared environmental (11.0%), and unique environmental (73.6%) influences. The odds of weak HGS significantly increased in the offspring of parents with weak HGS (odds ratio [OR], 1.69–3.10; P=0.027–0.038), especially in daughters (OR, 2.04–4.64; P=0.029–0.034).
Conclusion
HGS exhibits a familial correlation and significant heritable tendency in Korean adults. Therefore, Asian adults, especially women, who have parents with weak HGS, need to pay special attention to their muscle health with the help of healthy environmental stimuli.
- Calcium & Bone Metabolism
- Decreased Serum Level of Sclerostin in Older Adults with Sarcopenia
-
Seong Hee Ahn, Hee-Won Jung, Eunju Lee, Ji Yeon Baek, Il-Young Jang, So Jeong Park, Jin Young Lee, Eunah Choi, Yun Sun Lee, Seongbin Hong, Beom-Jun Kim
-
Endocrinol Metab. 2022;37(3):487-496. Published online May 27, 2022
-
DOI: https://doi.org/10.3803/EnM.2022.1428
-
-
3,177
View
-
142
Download
-
11
Web of Science
-
10
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader  ePub ePub
- Background
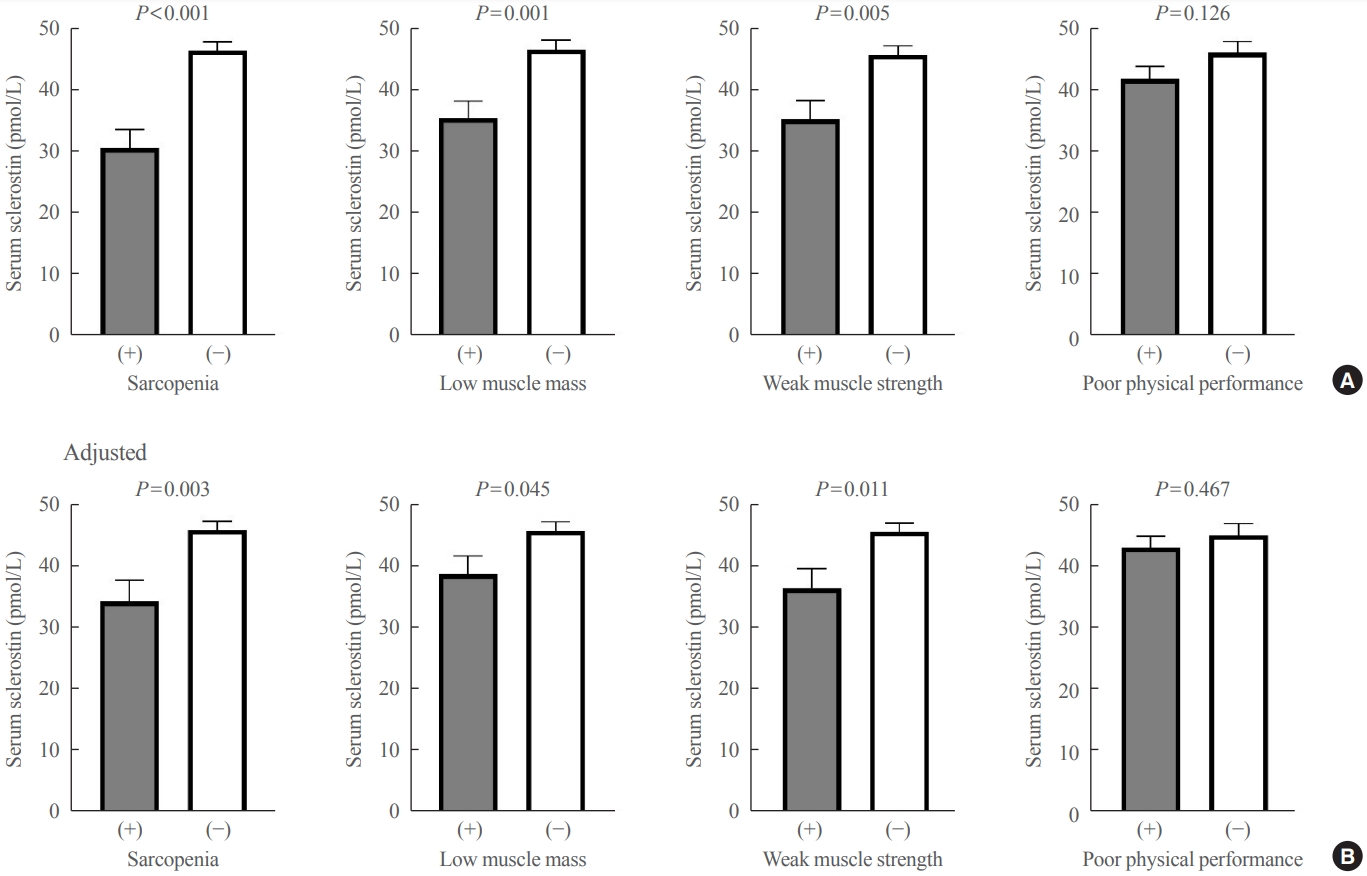
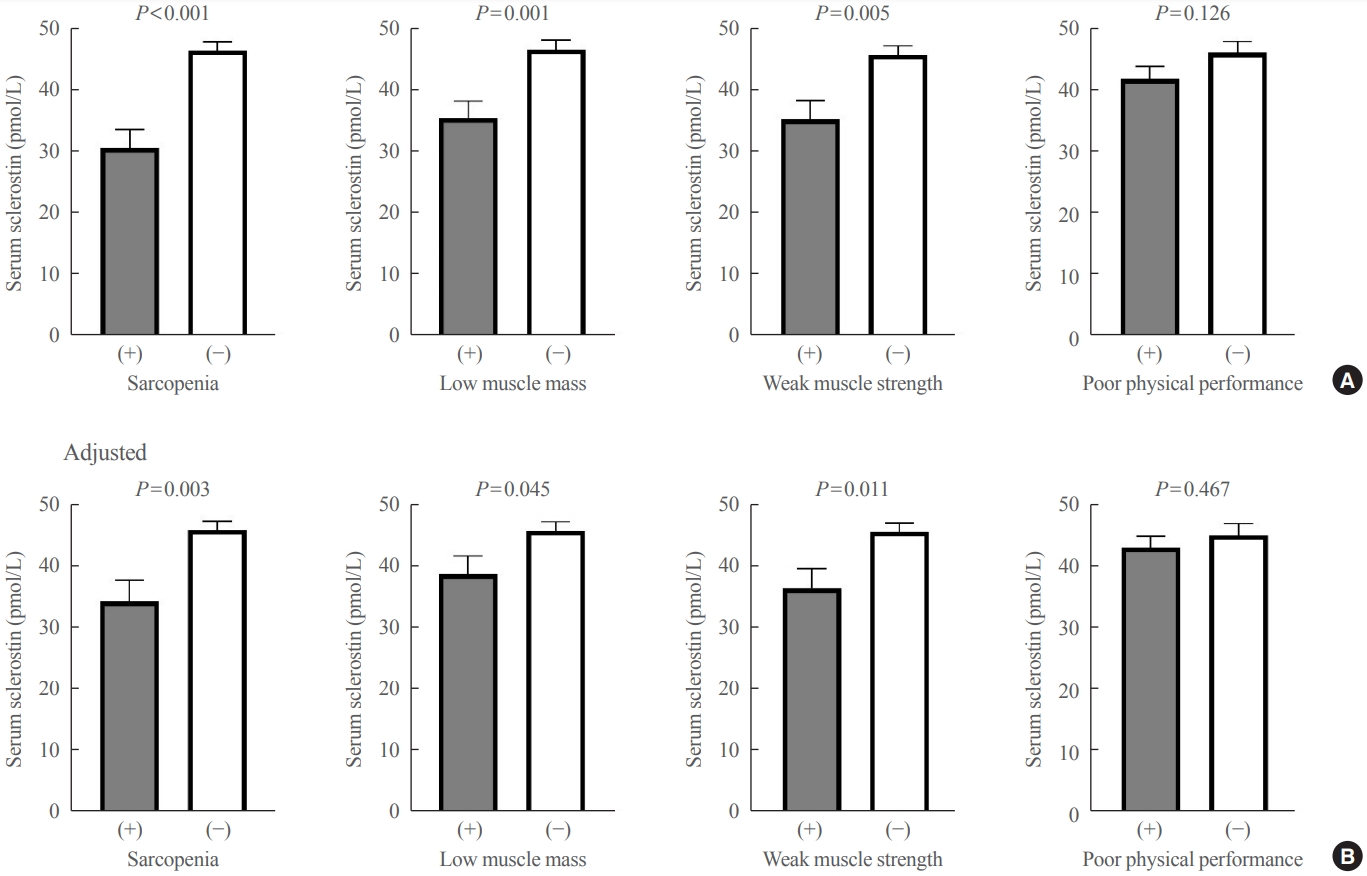
Although muscles and bones interact with each other through various secretory factors, the role of sclerostin, an osteocyte-secreted factor, on muscle metabolism has not been well studied. We investigated the levels of serum sclerostin in Korean older adults with sarcopenia.
Methods
Blood samples were collected from 129 participants who underwent evaluation of muscle mass and function in an outpatient geriatric clinic of a teaching hospital. Sarcopenia and related parameters were determined using cutoff values for the Asian population. Serum sclerostin levels were measured using an enzyme-linked immunosorbent assay.
Results
The mean age of the participants was 69.6 years, and 20 participants (15.5%) were classified as having sarcopenia. After adjusting for age, sex, and body mass index, serum sclerostin levels were significantly lower in participants with sarcopenia, low muscle mass, or weak muscle strength (P=0.003 to 0.045). Serum sclerostin levels were positively associated with skeletal muscle index and grip strength after adjusting for confounders (P=0.001 and P=0.003), whereas sarcopenic phenotype score showed a negative association (P=0.006). These increases in muscle mass and strength were also dose dependent as serum sclerostin levels increased (P for trends=0.003 and P for trends=0.015). Higher serum sclerostin levels were associated with lower odds ratio (ORs) for sarcopenia, low muscle mass, and weak muscle strength after adjusting for confounders (OR, 0.27 to 0.50; P<0.001 to 0.025).
Conclusion
Higher serum sclerostin levels were associated with a lower risk of sarcopenia, low muscle mass, and weak muscle strength in Korean older adults.
-
Citations
Citations to this article as recorded by  - Mechanism and physical activities in bone-skeletal muscle crosstalk
Zhonghan Zhao, Kai Yan, Qiao Guan, Qiang Guo, Can Zhao
Frontiers in Endocrinology.2024;[Epub] CrossRef - Musculoskeletal disorders and coronary artery disease —promising molecular markers: literature review
Viktoria N. Karetnikova, Anastasiya G. Neeshpapa, Evgenia I. Carpova, Olga L. Barbarash
CardioSomatics.2024; 15(1): 55. CrossRef - Determinants of bone mass in older adults with normal- and overweight derived from the crosstalk with muscle and adipose tissue
Carina O. Walowski, Catrin Herpich, Janna Enderle, Wiebke Braun, Marcus Both, Mario Hasler, Manfred J. Müller, Kristina Norman, Anja Bosy-Westphal
Scientific Reports.2023;[Epub] CrossRef - Role of the Osteocyte in Musculoskeletal Disease
Anika Shimonty, Lynda F. Bonewald, Fabrizio Pin
Current Osteoporosis Reports.2023; 21(3): 303. CrossRef - The role of sclerostin in lipid and glucose metabolism disorders
Hewen Jiang, Dijie Li, Ying Han, Nanxi Li, Xiaohui Tao, Jin Liu, Zongkang Zhang, Yuanyuan Yu, Luyao Wang, Sifan Yu, Ning Zhang, Huan Xiao, Xin Yang, Yihao Zhang, Ge Zhang, Bao-Ting Zhang
Biochemical Pharmacology.2023; 215: 115694. CrossRef - Cytokines and exosomal miRNAs in skeletal muscle–adipose crosstalk
Liu Guo, Menchus Quan, Weijun Pang, Yulong Yin, Fengna Li
Trends in Endocrinology & Metabolism.2023; 34(10): 666. CrossRef - Sclerostin: clinical insights in muscle–bone crosstalk
Antimo Moretti, Giovanni Iolascon
Journal of International Medical Research.2023;[Epub] CrossRef - Anti-sclerostin antibodies: a new frontier in fragility fractures treatment
Giovanni Iolascon, Sara Liguori, Marco Paoletta, Giuseppe Toro, Antimo Moretti
Therapeutic Advances in Musculoskeletal Disease.2023;[Epub] CrossRef - Sclerostin as a Putative Myokine in Sarcopenia
Hyon-Seung Yi
Endocrinology and Metabolism.2022; 37(3): 430. CrossRef - Organokines, Sarcopenia, and Metabolic Repercussions: The Vicious Cycle and the Interplay with Exercise
Giulia Minniti, Letícia Maria Pescinini-Salzedas, Guilherme Almeida dos Santos Minniti, Lucas Fornari Laurindo, Sandra Maria Barbalho, Renata Vargas Sinatora, Lance Alan Sloan, Rafael Santos de Argollo Haber, Adriano Cressoni Araújo, Karina Quesada, Jesse
International Journal of Molecular Sciences.2022; 23(21): 13452. CrossRef
- Obesity and Metabolism
- Metformin-Associated Lactic Acidosis: Predisposing Factors and Outcome
-
Min Ju Kim, Ju Young Han, Jun Young Shin, Shin Il Kim, Jeong Min Lee, Seongbin Hong, So Hun Kim, Moon Suk Nam, Yong Seong Kim
-
Endocrinol Metab. 2015;30(1):78-83. Published online March 27, 2015
-
DOI: https://doi.org/10.3803/EnM.2015.30.1.78
-
-
4,726
View
-
80
Download
-
28
Web of Science
-
28
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader
- Background
Metformin is considered the first choice oral treatment for type 2 diabetes patients in the absence of contraindications. Rarely, life-threatening complications associated with metformin treatment are seen in some patients with underlying diseases. The aim of this study was to further investigate the clinical profiles and risk factors for metformin-associated lactic acidosis (MALA) and the treatment modalities according to survival. MethodsTo identify MALA, we performed a retrospective study in seven diabetic patients who were taking metformin and had been diagnosed with lactic acidosis at Inha University Hospital between 1995 and 2012. For each patient, we recorded the age, sex, daily metformin dosage, laboratory test results, admission diagnosis, and risk factors. Also, concurrent conditions, treatment modalities, and outcomes were evaluated. ResultsSix patients had risk factors for lactic acidosis before admission. All patients had renal impairment on admission as a precipitating risk factor. Five patients survived and two patients died despite early renal replacement therapy. Older patients tended to have a poorer prognosis. ConclusionRenal function must be monitored in elderly type 2 diabetes mellitus patients with underlying diseases and conditions causing renal impairment who begin metformin treatment. Accurate recognition of MALA and initiation of renal replacement are essential for treatment.
-
Citations
Citations to this article as recorded by  - An Analysis of Clinical Outcomes of Exploratory Pediatric Metformin Ingestions Reported to the Texas Poison Center Network From 2011 to 2021
Shawn M. Varney, Sarah Watkins, Haylea Stuteville, Mark L. Winter, Han Tony Gao, Thomas G. Martin, Ryan P. Morrissey, Wayne R. Snodgrass, Brett A. Roth
Hospital Pharmacy.2024;[Epub] CrossRef - Causal association of metformin treatment with diverse cardiovascular diseases: a Mendelian randomization analysis
Kaiyuan Li, Peng Liu, Jun Ye, Miao Liu, Li Zhu
Aging.2024;[Epub] CrossRef - Metformin Treatment Reduces the Incidence of Rheumatoid Arthritis: A Two-Sample Mendelian Randomized Study
Jialin Liang, Yuanqing Cai, Jianan Zhang, Zhaopu Jing, Leifeng Lv, Guangyang Zhang, Rupeng Zhang, Ruiyu Liu, Kai Nan, Xiaoqian Dang
Journal of Clinical Medicine.2023; 12(7): 2461. CrossRef - PLGA-based microspheres loaded with metformin hydrochloride: Modified double emulsion method preparation, optimization, characterization, and in vitro evaluation
Priyanka Chauhan, Himanshu Paliwal, Chetan Singh Chauhan, Ankit Paliwal
Annales Pharmaceutiques Françaises.2023; 81(6): 997. CrossRef - Metformin-associated lactic acidosis: underlying multiple myeloma
Clara GOMES, Ana FERREIRA, Neuza SOARES, Vanessa CHAVES, Luís LEMOS, Sofia TAVARES, Marta COUTO
Gazzetta Medica Italiana Archivio per le Scienze Mediche.2022;[Epub] CrossRef - Metformin-associated lactic acidosis and factors associated with 30-day mortality
Kanin Thammavaranucupt, Boonchan Phonyangnok, Watanyu Parapiboon, Laddaporn Wongluechai, Watthikorn Pichitporn, Jirut Sumrittivanicha, Somnuek Sungkanuparph, Arkom Nongnuch, Kulapong Jayanama, Donovan Anthony McGrowder
PLOS ONE.2022; 17(8): e0273678. CrossRef - Metformin Associated Lactic Acidosis in Clinical Practice – A Case Series
Philipp Schädle, Otto Tschritter, Monika Kellerer
Experimental and Clinical Endocrinology & Diabetes.2021; 129(11): 842. CrossRef - Effect of continuous use of metformin on kidney function in diabetes patients with acute myocardial infarction undergoing primary percutaneous coronary intervention
Qi Yu, Jia-Jia Zhu, Wen-Xian Liu
BMC Cardiovascular Disorders.2020;[Epub] CrossRef - Metformin: current clinical applications in nondiabetic patients with cancer
Kailin Chen, Yajun Li, Zhen Guo, Yong Zeng, Wei Zhang, Hui Wang
Aging.2020; 12(4): 3993. CrossRef - Specifics of diabetes in old age
Markéta Kubíčková
Interní medicína pro praxi.2019; 21(4): 223. CrossRef - The Association between Metformin Therapy and Lactic Acidosis
Isabelle H. S. Kuan, Ruth L. Savage, Stephen B. Duffull, Robert J. Walker, Daniel F. B. Wright
Drug Safety.2019; 42(12): 1449. CrossRef - Metformin overdose: A serious iatrogenic complication—Western France Poison Control Centre Data Analysis
Alexandre Stevens, Jean‐François Hamel, Ali Toure, Samy Hadjadj, David Boels
Basic & Clinical Pharmacology & Toxicology.2019; 125(5): 466. CrossRef - Risk of Metformin-Associated Lactic Acidosis (MALA) in Patients After Gastric Bypass Surgery
Laura N. Deden, Edo O. Aarts, Stephanie C. W. Aelfers, Marcel M. G. J. van Borren, Ignace M. C. Janssen, Frits J. Berends, Hans de Boer
Obesity Surgery.2018; 28(4): 1080. CrossRef - Metformin-related lactic acidosis: Case report
Jesús Salvador Sánchez-Díaz, Enrique Monares-Zepeda, Enrique Antonio Martínez-Rodríguez, Jorge Samuel Cortés-Román, Oscar Torres-Aguilar, Karla Gabriela Peniche-Moguel, Susana Patricia Díaz-Gutiérrez, Eusebio Pin-Gutiérrez, Gerardo Rivera-Solís, Rosalba C
Colombian Journal of Anesthesiology.2017; 45(4): 353. CrossRef - Metformin-related lactic acidosis: Case report☆
Jesús Salvador Sánchez-Díaz, Enrique Monares-Zepeda, Enrique Antonio Martínez-Rodríguez, Jorge Samuel Cortés-Román, Oscar Torres-Aguilar, Karla Gabriela Peniche-Moguel, Susana Patricia Díaz-Gutiérrez, Eusebio Pin-Gutiérrez, Gerardo Rivera-Solís, Rosalba C
Colombian Journal of Anesthesiology.2017; 45(4): 353. CrossRef - Association between Metformin Use and Risk of Lactic Acidosis or Elevated Lactate Concentration in Type 2 Diabetes
Eun Young Lee, Sena Hwang, Yong-ho Lee, Seo Hee Lee, Young Mi Lee, Hua Pyong Kang, Eugene Han, Woonhyoung Lee, Byung-Wan Lee, Eun Seok Kang, Bong Soo Cha, Hyun Chul Lee
Yonsei Medical Journal.2017; 58(2): 312. CrossRef - Hypoglycemia and severe lactic acidosis in a dog following metformin exposure
Nicole Barrella, Beth Eisenberg, Stephanie Nicole Simpson
Clinical Case Reports.2017; 5(12): 2097. CrossRef - Acidosis láctica por metformina: reporte de caso
Jesús Salvador Sánchez-Díaz, Enrique Monares-Zepeda, Enrique Antonio Martínez-Rodríguez, Jorge Samuel Cortés-Román, Oscar Torres-Aguilar, Karla Gabriela Peniche-Moguel, Susana Patricia Díaz-Gutiérrez, Eusebio Pin-Gutiérrez, Gerardo Rivera-Solís, Rosalba C
Revista Colombiana de Anestesiología.2017; 45(4): 353. CrossRef - Towards natural mimetics of metformin and rapamycin
Alexander Aliper, Leslie Jellen, Franco Cortese, Artem Artemov, Darla Karpinsky-Semper, Alexey Moskalev, Andrew G. Swick, Alex Zhavoronkov
Aging.2017; 9(11): 2245. CrossRef - Metformin-Associated Lactic Acidosis
Martin R. Hevesy
Advanced Emergency Nursing Journal.2017; 39(1): 26. CrossRef - Metformin associated lactic acidosis (MALA): clinical profiling and management
Alessandra Moioli, Barbara Maresca, Andrea Manzione, Antonello Maria Napoletano, Daniela Coclite, Nicola Pirozzi, Giorgio Punzo, Paolo Menè
Journal of Nephrology.2016; 29(6): 783. CrossRef - Risk assessment and management of post-transplant diabetes mellitus
Eugene Han, Myoung Soo Kim, Yu Seun Kim, Eun Seok Kang
Metabolism.2016; 65(10): 1559. CrossRef - Temporal trends in the use of antidiabetic medicines: a nationwide 9-year study in older people living in New Zealand
Prasad S. Nishtala, Mohammed Saji Salahudeen
Therapeutic Advances in Drug Safety.2016; 7(5): 184. CrossRef - Metformin-associated lactic acidosis: Current perspectives on causes and risk
Ralph DeFronzo, G. Alexander Fleming, Kim Chen, Thomas A. Bicsak
Metabolism.2016; 65(2): 20. CrossRef - Lactic acidosis and the relationship with metformin usage
Weiyi Huang, Ronald L. Castelino, Gregory M. Peterson
Medicine.2016; 95(46): e4998. CrossRef - Metformin stimulates IGFBP-2 gene expression through PPARalpha in diabetic states
Hye Suk Kang, Ho-Chan Cho, Jae-Ho Lee, Goo Taeg Oh, Seung-Hoi Koo, Byung-Hyun Park, In-Kyu Lee, Hueng-Sik Choi, Dae-Kyu Song, Seung-Soon Im
Scientific Reports.2016;[Epub] CrossRef - Metformin-associated lactic acidosis: time to let it go?
Chantal Mathieu
Journal of Diabetes and its Complications.2015; 29(8): 974. CrossRef - Metformin: risk-benefit profile with a focus on cancer
Nicoletta Provinciali, Matteo Lazzeroni, Massimiliano Cazzaniga, Franco Gorlero, Barbara K Dunn, Andrea DeCensi
Expert Opinion on Drug Safety.2015; 14(10): 1573. CrossRef
|